Insurers cut back GLP-1 coverage as demand soars: Found study

As demand surges for GLP-1 therapies, insurers are pulling back on coverage, according to new data from obesity care provider Found. | Sarah Jones Simmer, CEO of Found, said that the trends are likely the result of irresponsible prescribing for recreational reasons causing the pendulum to swing "all the way in the other direction," and it's leading to patients who have genuine medical need struggling to access these therapies.
Why Won't Your Company Pay for Weight-Loss Drugs Like Wegovy

The Doctor Prescribed an Obesity Drug. Her Insurer Called It 'Vanity.' - The New York Times

Why Won't Your Company Pay for Weight-Loss Drugs Like Wegovy
/sites/default/files/styles/embed_xxl/p

Blog_ USPM Blog (2024)

Focus: US diabetes patients face delays as insurers tighten Ozempic coverage

Ozempic vs. Metformin: Which Is Right for You?

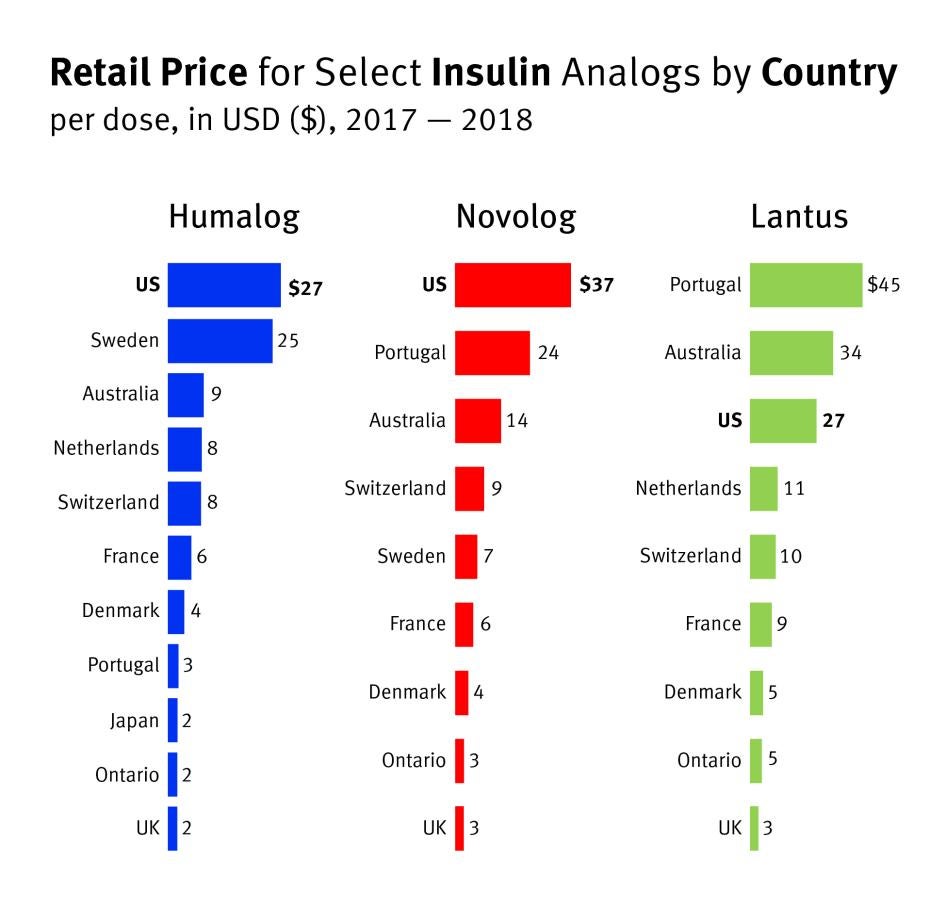
As the market for new weight loss drugs soars, people with diabetes pay the price
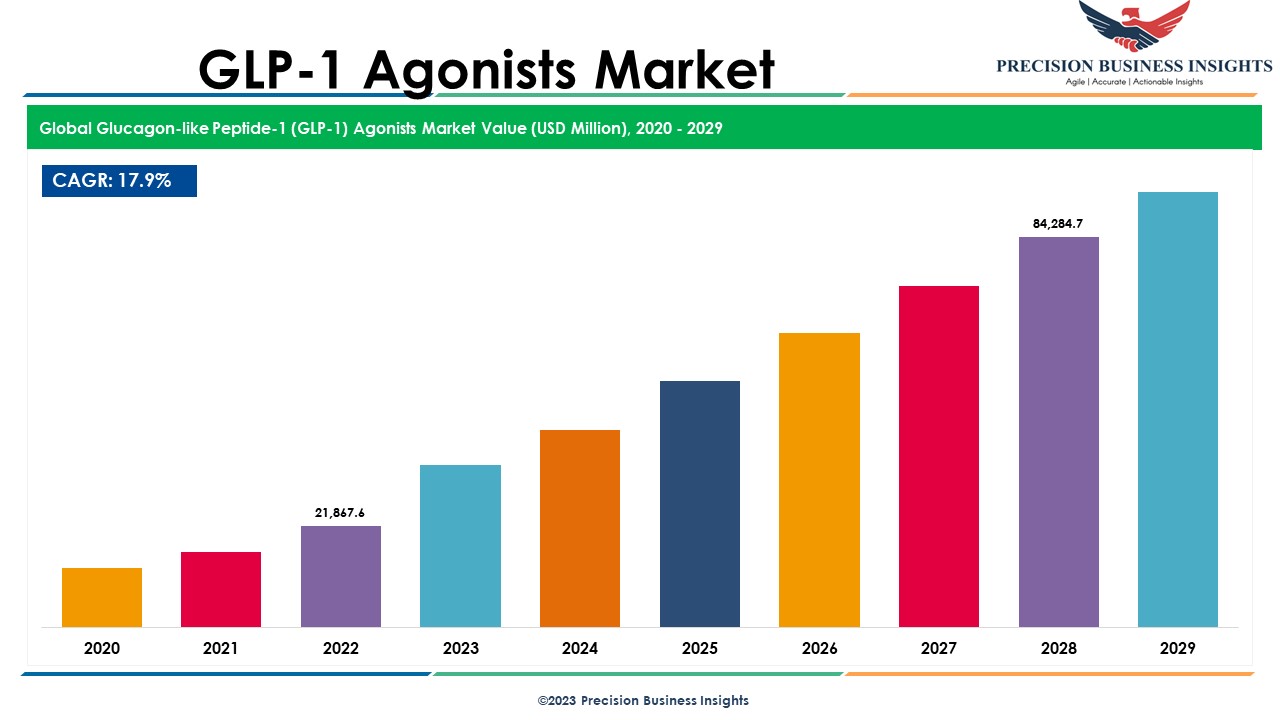
GLP-1 Agonists Market Share, Size, Growth Insights 2030