Mixed methods feasibility and usability testing of a childhood obesity risk estimation tool, BMC Public Health
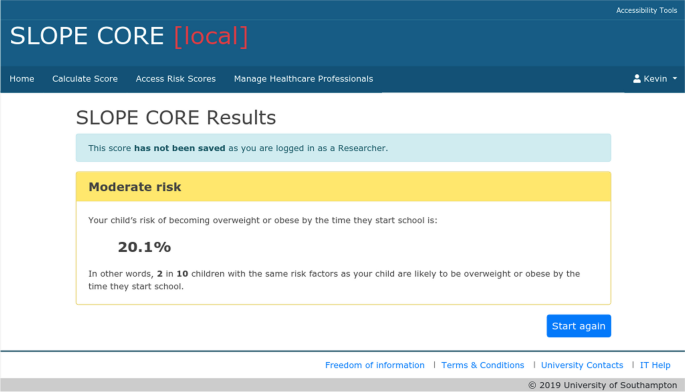
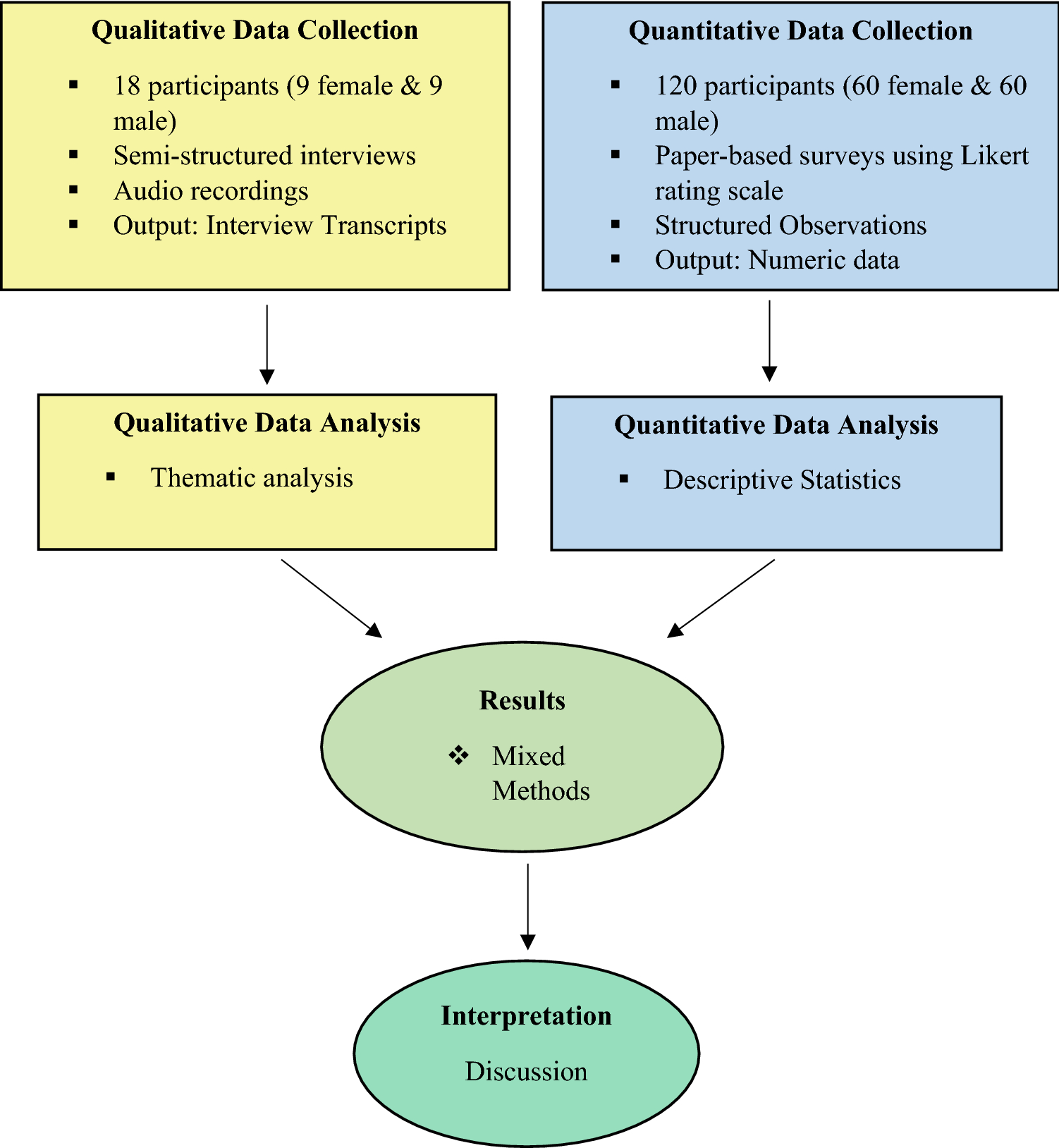
Background A Childhood Obesity Risk Estimation tool (SLOPE CORE) has been developed based on prediction models using routinely available maternity and early childhood data to estimate risk of childhood obesity at 4–5 years. This study aims to test the feasibility, acceptability and usability of SLOPE CORE within an enhanced health visiting (EHV) service in the UK, as one context in which this tool could be utilised. Methods A mixed methods approach was used to assess feasibility of implementing SLOPE CORE. Health Visitors (HVs) were trained to use the tool, and in the processes for recruiting parents into the study. HVs were recruited using purposive sampling and parents by convenience sampling. HVs and parents were invited to take part in interviews or focus groups to explore their experiences of the tool. HVs were asked to complete a system usability scale (SUS) questionnaire. Results Five HVs and seven parents took part in the study. HVs found SLOPE CORE easy to use with a mean SUS of 84.4, (n = 4, range 70–97.5) indicating excellent usability. Five HVs and three parents took part in qualitative work. The tool was acceptable and useful for both parents and HVs. Parents expressed a desire to know their child’s risk of future obesity, provided this was accompanied by additional information, or support to modify risk. HVs appreciated the health promotion opportunity that the tool presented and felt that it facilitated difficult conversations around weight, by providing ‘clinical evidence’ for risk, and placing the focus of the conversation onto the tool result, rather than their professional judgement. The main potential barriers to use of the tool included the need for internet access, and concerns around time needed to have a sensitive discussion around a conceptually difficult topic (risk). Conclusions SLOPE CORE could potentially be useful in clinical practice. It may support targeting limited resources towards families most at risk of childhood obesity. Further research is needed to explore how the tool might be efficiently incorporated into practice, and to evaluate the impact of the tool, and any subsequent interventions, on preventing childhood obesity.

Delaware Journal of Public Health - May 2022 by Delaware Academy of Medicine and the Delaware Public Health Association - Issuu

Flow diagram showing the eligible sample (n = 8003) for this
Information, Free Full-Text
PDF) Process evaluation of the Yéego! Program to increase healthy eating and gardening among American Indian elementary school children
Nutrients, Free Full-Text
Perception, environmental determinants, and health complications of excess weight in India: a mixed methods approach

Delaware Journal of Public Health, Chronic Disease, Part 1 by Delaware Academy of Medicine and the Delaware Public Health Association - Issuu
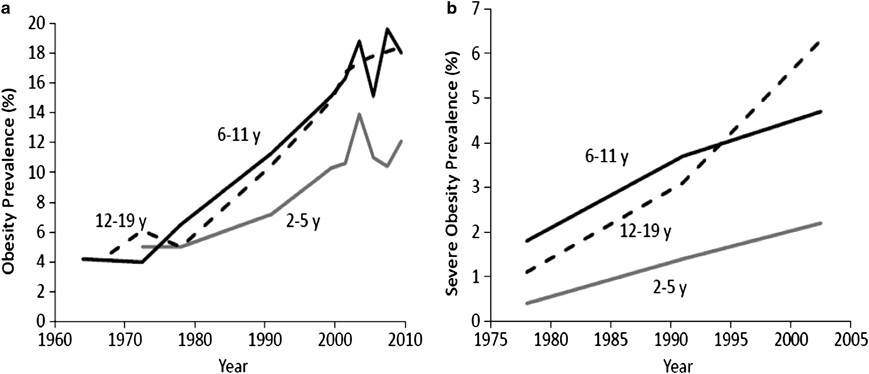
An evolving scientific basis for the prevention and treatment of pediatric obesity

Childhood Obesity Evidence Base Project: A Systematic Review and Meta- Analysis of a New Taxonomy of Intervention Components to Improve Weight Status in Children 2–5 Years of Age, 2005–2019

BMC Public Health 1/2015